Endometriosis is a chronic and often debilitating condition that affects an estimated 10% of women and individuals assigned female at birth, yet it takes an average of 7 to 10 years to receive a proper diagnosis. This delay can have significant physical, emotional, and social consequences for those affected.
But why does it take so long to diagnose endometriosis? The answer lies in a combination of medical misconceptions, symptom overlap, lack of awareness, and limitations in diagnostic tools.
1. Endometriosis Symptoms Overlap with Other Conditions
One of the biggest challenges in diagnosing endometriosis is that its symptoms, such as severe menstrual pain, chronic pelvic pain, painful intercourse, digestive issues, and fatigue, overlap with many other conditions. Disorders like irritable bowel syndrome (IBS), pelvic inflammatory disease (PID), interstitial cystitis, and even normal menstrual cramps can mimic endometriosis, leading doctors to misdiagnose or dismiss symptoms.
Since endometriosis does not always present itself in a predictable way, many patients are shuffled between gynaecologists, gastroenterologists, urologists, and pain specialists before they finally receive an accurate diagnosis. This results in years of unnecessary treatments, tests, and suffering.
2. Societal Normalisation of Menstrual Pain
Many women are conditioned to believe that painful periods are normal. From adolescence, they are often told that period pain is just a part of life and they should “tough it out” with over-the-counter painkillers. Because of this, many people with endometriosis delay seeking medical attention, thinking their symptoms are exaggerated or not serious enough.
Even when they do seek help, many doctors downplay their complaints, prescribing birth control or painkillers without further investigation. This dismissal leads to delayed diagnosis and prolonged suffering.
3. Lack of Non-Invasive Diagnostic Tools
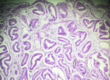
Unlike other medical conditions that can be diagnosed with a simple blood test or imaging scan, endometriosis cannot be definitively diagnosed without surgery. While ultrasounds and MRIs may detect large endometriotic cysts, they often miss superficial lesions or deep infiltrating endometriosis.
The gold standard for diagnosing endometriosis is laparoscopy, a minimally invasive surgical procedure in which a camera is inserted into the abdomen to look for endometriotic lesions. However, surgery is expensive, invasive, and not always accessible, making many doctors hesitant to recommend it as a first step. Instead, they often experiment with treatments, further delaying an official diagnosis.
4. Gender Bias in Medical Research
Medical research has historically focused more on men’s health issues, leaving many women’s health conditions underfunded and poorly understood. Endometriosis is no exception. There is a lack of awareness and education about the disease among healthcare providers, and many doctors still hold outdated beliefs that it only affects older women or those with fertility issues.
This medical bias contributes to misdiagnosis and dismissive attitudes, forcing patients to advocate strongly for themselves, sometimes for years, before receiving proper care.
5. Slow Progress in Treatment and Awareness
Despite its prevalence, endometriosis is still poorly understood, and there is no cure. Treatment mainly consists of pain management, hormonal therapy, and surgery, none of which guarantee long-term relief. The lack of research funding, combined with limited public awareness, means that progress in improving diagnosis and treatment has been frustratingly slow.
However, awareness campaigns and advocacy groups are working to change this narrative by educating healthcare professionals and encouraging earlier screening.
Conclusion: The Need for Change
The long delay in diagnosing endometriosis is a serious healthcare issue that leaves millions of people suffering unnecessarily. To improve early diagnosis, we need better medical training, increased awareness, more research funding, and improved diagnostic methods. More importantly, patients need to be believed and taken seriously when they report their symptoms.
If you suspect you have endometriosis, it is crucial to advocate for yourself, seek a second opinion if necessary, and push for diagnostic tests. Early intervention can make a significant difference in managing symptoms and preserving quality of life.